Category Archives: Post Transplant Depression
Post Transplant Depression, It’s Common and There’s Help!
By Bob Aronson
 Having suffered from post transplant depression myself, I know of what I speak. It hits you like a sledge hammer and keeps pounding away. The pain isn’t physical, it’s emotional and it can be intense, so intense that some consider taking their own lives. Worst of all, few if any of your family and friends understand and some become impatoemt. dsksdddddddddddddlkkkkkkkkkkkkkksddddddddddddddddddddddddddddddddddddddddddddddddddlddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddccsssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssjnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssss with your continued mood swings. They don’t even have the most basic understanding of the disease. While their intentions are good, their advice usually isn’t. They will say things like, “Buck up, My God your’re alive, you got a new heart and you’re alive.” To that I can only say, “I would be happy to buck up if I could, but I can’t. Noone would choose to live like this You can feel useless, unnecessary, irrelevant and totally without purpose. Some patients even feel suicidal, but it doesn’t have to be that way. There is help.
Having suffered from post transplant depression myself, I know of what I speak. It hits you like a sledge hammer and keeps pounding away. The pain isn’t physical, it’s emotional and it can be intense, so intense that some consider taking their own lives. Worst of all, few if any of your family and friends understand and some become impatoemt. dsksdddddddddddddlkkkkkkkkkkkkkksddddddddddddddddddddddddddddddddddddddddddddddddddlddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddccsssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssjnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssss with your continued mood swings. They don’t even have the most basic understanding of the disease. While their intentions are good, their advice usually isn’t. They will say things like, “Buck up, My God your’re alive, you got a new heart and you’re alive.” To that I can only say, “I would be happy to buck up if I could, but I can’t. Noone would choose to live like this You can feel useless, unnecessary, irrelevant and totally without purpose. Some patients even feel suicidal, but it doesn’t have to be that way. There is help.
If there’s one message you should take away from this blog, it is this. Depression is not your fault, you did not cause it and therefore you alone can not fix it. “Cheer up, look at the bright side,” may sound like good advice but it isn’t because it assumes you decided to feel lousy. Who on earth would choose to be depressed? It is sad, but true that sometimes even the people closest to you don’t understand. They continue to hold on to the belief that you can snap out of it if you really want to. The reality of depression just isn’t that simple. Frankly, it is very, very complex and takes highly skilled and trained professionals to help you find your way back to the sunny side of the street.
Unfortunately if you have had or if you are going to have an organ transplant, chances are good that you might fall victim to post transplant depression. Estimates of how many patients become depressed following an organ transplant range from 10 percent all the way up to 50%, but no matter what the percentage the fact is that some people will have serious emotional struggles following their transplant.
One can easily ask, “Depression? Why on earth would anyone be depressed after their life has been saved by the donor/transplantation process?” Well, there are a number of reasons, chief among them is the haunting feeling that someone had to die in order for you to live. The fact is, the person who died, would have died anyway whether they were an organ donor or not and if they were, someone might gain new life as a result, but that’s logic and logic alone cannot solve the problem and help the patient. Besides, there are other issues that contribute to depression like:
- Living with the psychological highs and lows that are sometimes
 caused by immunosuppressives such as corticosteroids
caused by immunosuppressives such as corticosteroids - The steroids you take can have the effect of a mood amplifier. In the first few weeks, especially, when the doses are highest, the medicine will wind you up and make it hard to sleep. The sudden changes in the family — and in your behavior — can be extreme.
- Managing a complex post-transplant regimen that encompasses: (1) multiple meds and schedules, (2) monitoring vital signs, (3) exercise and dietary requirements, (4) regular medical evaluations and lab tests, and (5) lifestyle restrictions on smoking, alcohol, and other potentially harmful substances
- Major life alterations such as transitioning from being critically ill or dying patients and family caregivers to roles that are more wellness-focused)
- Coping with new and taxing financial and economic issues like the cost of transplant surgery, hospital stays, follow-up care, cost of drugs and health insurance.
To some that list of changes is so overwhelming as to be nearly impossible to manage. Some have been seriously ill for such a very long time and so focused on dying that they cannot adjust to an attitude that centers on life and living. What is even worse is that unless the patient is getting professional psychiatric help he or she may not be able to identify a single stressor that brought on their depressed state.
Simply put, depression is a mood disorder that causes a persistent feeling of sadness and loss of interest in those things that had been of great importance. It affects how you feel, think and behave and can lead to a variety of problems. Day to day activities become ponderous and boring and patients sometimes feel their lives are not worth living.
Depression isn’t just feeling “down” and you can’t just “snap out of it.” It can require long-term treatment with either medication, psychological counseling or a combination of the two. Above all you must know that suffering from depression is not a personal weakness. You didn’t bring it on and will power alone cannot defeat it.
Depression can occur once or several times in a lifetime and according to the Mayo Clinic (http://tinyurl.com/ouory9u) the symptoms can appear all day, every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Changes in appetite — often reduced appetite and weight loss, but increased cravings for food and weight gain in some people
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or blaming yourself for things that aren’t your responsibility
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Other people may feel generally miserable or unhappy without really knowing why. http://tinyurl.com/lgsq8hm
Health Concerns
(Material gathered here comes from several sources primary among them is UNOS (the United Network for Organ Sharing).
What happens after transplantation depends on the organ transplanted and the recipient’s specific medical situation. Most patients recover fully, return to work and resume a normal, active life after receiving a new organ. However, there is a possibility of developing unrelated health problems after transplantation. That’s why it is important to work closely with your doctor concerning your overall wellness, as well as regarding the following health concerns:
Anxiety and Depression
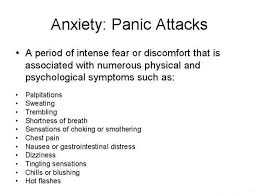 Patients and their families face a new lifestyle after transplantation that may cause them to feel nervous, stressed or depressed. Because emotional and psychological support is a continuing process, ask your social worker about counseling services that can help you and your family deal with these changes. Professionals can help you work through concerns about your self-image; mood swings; job planning; rehabilitation; family stresses, such as parent-child conflicts, marital conflict or changes in sexual functioning; and financial concerns, such as questions about Medicare, disability or insurance. Any and all of the following can contribute to your depression and/or anxiety.
Patients and their families face a new lifestyle after transplantation that may cause them to feel nervous, stressed or depressed. Because emotional and psychological support is a continuing process, ask your social worker about counseling services that can help you and your family deal with these changes. Professionals can help you work through concerns about your self-image; mood swings; job planning; rehabilitation; family stresses, such as parent-child conflicts, marital conflict or changes in sexual functioning; and financial concerns, such as questions about Medicare, disability or insurance. Any and all of the following can contribute to your depression and/or anxiety.
Diabetes
Some anti-rejection medicines are known to cause high blood sugar. Although it is typically a temporary condition after transplantation, it is more common in patients who have a family history of diabetes and patients who are overweight. It can be controlled by reducing the dose of a patient’s anti-rejection medicines or changing medications all together.
GI Upset
GI (gastrointestinal) or stomach upset is also a common complaint after a transplant. Patients on steroid therapy may be at an increased risk of developing ulcers due to increased hydrochloric acid from the stress of the procedure. Treatment of GI upset may include one or a combination of drugs that reduce acid production. In addition, people with GI upset should take several steps to reduce symptoms, including:
- Reducing the intake of caffeine, alcohol and over-the-counter medications that cause GI upset.
- Eliminating carbonated drinks can help
- And it sometimes helps to take your meds with food to decrease irritation.
Gout
Gout is a painful and potentially disabling form of arthritis. Diagnosing gout can be difficult and treatment plans vary based on a patient’s existing medical problems and medications. Often Gout will show up in the big toe and it is very painful. Sometimes even a bedsheet touching the Gout area will result in extreme pain.
High Cholesterol
Many immunosuppressant drugs can contribute to high cholesterol. This condition therefore affects many transplant recipients. When a patient develops high cholesterol, blood vessels, including the ones attached to the transplanted organ, become clogged, which affects the flow of blood. This slowing of blood flow can affect the success of your transplant and may even lead to heart disease. It is important to talk to your doctor about how to reduce the risk factors of heart disease, including controlling your cholesterol.
Hypertension
Hypertension, or high blood pressure, is common immediately after
transplant. Certain anti-rejection medications, as well as the original disease, all can contribute to hypertension. Treatment of hypertension may include one or a combination of drugs, and often, as anti-rejection medicines are tapered to a maintenance dose, hypertension may decrease. Talk to your doctor about what’s right for you and how to avoid high blood pressure.
Sexual Relations
Sexual concerns after transplantation are commonly experienced, yet seldom discussed or addressed during evaluation. It is therefore very important to talk with your doctor about your sexual history and concerns.
However, sexual function and interest can be related to how well your body has accepted your new organ and how realistic your expectations were for life after your transplant. A counselor can also help a couple understand the difference between pre- and post-transplant problems. Often, support groups can be very helpful in this regard.
Additionally, in sexual relations, as in all issues, recipients must remember that they are immune suppressed and subject to many kinds of infections. In fact, some infections in recently transplanted patients can be potentially life threatening. Consequently, it is important to consider the following points:
- The sharing of saliva during kissing can expose both partners to active diseases, such as colds or other viruses.
- Condoms don’t prevent diseases that are spread by contact between the area surrounding the penis and external genitals.
- The risk of contracting infectious diseases though oral sex is possible, especially if ejaculation occurs or if there are any sores or wounds on either partner.
Shingles
People with weakened immune systems, such as transplant recipients treated with immunosuppressive drugs, risk developing shingles. Shingles is a painful infection of the central nervous system caused by the Varicella virus that causes a blistering rash and severe burning pain, tingling or extreme sensitivity to the skin and is usually limited to one side of the body. The severity and duration of an attack of shingles can be significantly reduced by immediate treatment with antiviral drugs. You should also ask your doctor about getting the Shingles vaccine.
Sometimes our own irresponsible behavior is responsible for feelings of depression or inadequacy. It has been established that noncompliance appears to be relatively common during the first several years after transplantation. That means some patients just don’t take the right amount of medication at the right time, if they take it at all. Furthermore, compliance in most areas of the medical regimen worsens over the first year after the transplant just as it does for most patients who begin new medical therapies. For example:
- Up to 20% of heart transplant recipients and 50% of kidney transplant recipients have been found to be noncompliant with prescribed immunosuppressant medications during a given 12-month period in the early post-transplant years
- 5% to 26% of heart transplant recipients smoke at least once after being transplanted; no study has determined what proportion of these patients become regular smokers.
- 11% to 48% of liver transplant recipients return to some level of alcohol consumption during the first year post-transplantation.
| As a result of noncompliance patients are likely to experience rejection symptoms or actual rejection and, of course when this happens patients experience anxiety and/or depression. http://tinyurl.com/qjlc48n
Treatment options |
 Researchers at Henry Ford Hospital have found that emotional closeness between transplant patients and their caregivers helps reduce depression and anxiety after surgery. While this study was about liver transplant patients, it is likely that the conclusions probably have universal application.
Researchers at Henry Ford Hospital have found that emotional closeness between transplant patients and their caregivers helps reduce depression and anxiety after surgery. While this study was about liver transplant patients, it is likely that the conclusions probably have universal application.
“People with close networks and good support recover faster after liver transplant and have less depression and anxiety at six months after transplant,” says Anne Eshelman, Ph.D., Henry Ford Health System Behavioral Health Services, lead author of the study.
“These findings suggest caregiving relationships as a target for psycho-therapeutic intervention among patients with end-stage liver disease.”
Study results were presented at the International Congress of Behavioral Medicine in Washington D.C., held by the International Society of Behavioral Medicine and the Society of Behavioral Medicine.
The study looked at 74 liver transplant surgery candidates and their primary caregivers. Transplant patients were surveyed before surgery and at a six-month follow-up. Caregivers rated the degree of closeness they felt in their relationship to the patient.
The sample was divided into groups with caregivers reporting maximum closeness or less closeness.
For patients with end-stage liver disease, depression and anxiety improve after liver transplant, but the study found that these changes are not as great for individuals with emotionally distant caregiving relationships.
“If you live with someone who loves you, the quality of care they provide may be much better, they may be more encouraging, you may want to please them and recuperate faster so you can spend quality time with them,” says Dr. Eshelman. “Caregivers who are not close, may provide the basic requirements, but don’t help give someone a reason to live and look to the future.”
The study results also suggested that emotional closeness was critical for affective improvement in men, but less so for women, though interpretation is limited by a small sample size, explained Dr. Eshelman.
“Men who had adequate number of support people, but did not have close support, were still depressed and anxious at follow up, compared to those who had closer support,” says Dr. Eshelman. “Other literature shows that women have wider support, more friends and family they are connected to than men, and if the primary support person is not that close, they probably rely on the other people such as girlfriends.”
The study was funded by Henry Ford Transplant Institute. http://tinyurl.com/q4bwqzs
Treatments for Depression
From Web MD
If you are diagnosed with depression, here’s some good news: Excellent treatment options are available to you.
Many people use a combination of treatments, such as medication and psychotherapy. For depression that doesn’t respond to standard treatment, non-drug approaches can be effective, either alone or used with other treatments.
Learn more here about the most common approaches to treating depression.
Talk Therapy for Depression
Talking with a trained therapist is one of the best treatments. Some people choose to be in therapy for several months to work on a few key issues. Other people find it helpful to continue in therapy for years, gradually working through larger problems. The choice is up to you and your therapist. Here are some common types of therapy:
- Cognitive behavioral therapyhelps you see how behaviors and the way you think about things plays a role in your depression. Your therapist will help you change some of these unhealthy patterns.
- Interpersonal therapyfocuses on your relationships with other people and how they affect you. Your therapist will also help you pinpoint and change unhealthy habits.
- Problem-solving therapyfocuses on the specific problems you face and helps you find solutions.
Medicines for Depression
Medicines are the other key treatment for depression. If one antidepressant doesn’t work well, you might try a similar one or a different kind. Your doctor might also try changing the dose. In some cases, he or she might recommend taking more than one medication for your depression. There are now many different antidepressants that your doctor can choose from. The entire listing can be seen here: http://tinyurl.com/p4yaq4b
doesn’t work well, you might try a similar one or a different kind. Your doctor might also try changing the dose. In some cases, he or she might recommend taking more than one medication for your depression. There are now many different antidepressants that your doctor can choose from. The entire listing can be seen here: http://tinyurl.com/p4yaq4b
Just keep in mind that recovery is a process that may need constant adjustment and takes time.
-0-
Bob Aronson of Bob’s Newheart is a 2007 heart transplant recipient, the founder of Facebook’s over 4,200 member Organ Transplant Initiative (OTI) and the author of most of these donation/transplantation blogs. You may comment in the space provided or email your thoughts to me at bob@baronson.org. And – please spread the word about the immediate need for more organ donors. There is nothing you can do that is of greater importance. If you convince one person to be an organ and tissue donor you may save or positively affect over 60 lives. Some of those lives may be people you know and love. You can register to be a donor at http://www.donatelife.net. It only takes a few minutes. Then, when registered, tell your family about your decision so there is no confusion when the time comes.
Post Transplant Depression — It’s Real and it’s Treatable
Early in July of 1995 I collapsed in a parking garage, got up, dragged myself to the car and drove to an emergency room. After a Battery of tests I was told I had dilated cardiomyopathy and would someday need a heart transplant. In simple terms cardiomyopathy is a weakening of the heart muscle that causes it to pump out less blood. The less it pumps out, the more it retains and the more it retains the bigger it gets. As your pumping capacity goes down the heart is forced to store more blood so it grows even more. Finally, when the pumping function is almost negligible and the heart can’t grow any more you die. It is called end-stage cardiomyopathy and it took me 12 years to get there, 12 years of continuous declining health, 12 years of knowing I was dying, 12 years of worrying about it. And…I was 12 years older, 68, and that doesn’t help when you need a heart transplant.
Does that sound depressing? Well it was but it was nowhere near as depressing as what I suffered after the transplant. “So,” you say, “Why would you be depressed after a transplant, you just got a new lease on life you should be happy.” And if you said that, you’d be right, we should be happy but a very large number of transplant patients aren’t. Some even become suicidal. It wasn’t until four years after my transplant that I was finally free of depression.
Before we discuss why transplant patients get depressed, let’s talk a about what depression is, how to identify it and how can affect your life. Clinical depression can affect every part of your life…your ability to sleep, eat, work, and get along with others can be severely affected. Depression can ruin self-esteem and turn simple tasks like getting dressed and taking a shower into major struggles. People who suffer from depression can lose interest in things that used to excite them and put a dark and gloomy cloud over everyday life. It cannot be willed away and you can’t ignore it. There’s a lot that can be done to treat depression but the first step is to admit that you have a problem and that is not always easy. Depression like other diseases has symptoms which include:
- Decreased energy, fatigue
- Loss of interest in things that were once enjoyed, including sex
- Insomnia or sleeping too much, not wanting to get up
- Loss of appetite, or overeating
- Feelings of hopelessness
- Pessimistic about most things
- Feeling helpless and worthless
- Thoughts of death or suicide, or suicide attempts
If you have any of these symptoms you should get immediate medical attention but if you are still not sure, take this on-line test as a kind of second opinion. http://www.mayoclinic.com/health/depression/MH00103_D
Back to transplant patients and depression. I can only speak for myself but I have spoken with many transplant patients who have shared in my experiences. When I awoke after transplant surgery and the anesthesia wore off I felt a euphoria that defies description. Maybe it was realizing that I had survived the surgery or maybe it was the pain killers and residual effects of the anesthesia but I had this feeling of complete and total relief. If one can really achieve serenity I had at that moment. I have not experienced anything like it since. It didn’t last very long.
Anyone who knew me prior to my surgery will tell you that I have always been very outgoing, friendly, upbeat, optimistic and full of energy. That was my natural state but heart transplant surgery and the events surrounding it changed all that. After 9 days in the hospital I was released to go home but I was very weak, had little or no energy, and felt like I was no longer of any use to anyone. I had energy, no appetite, no sense of humor, no personality … nothing. All I wanted to do was sit in my recliner in a dark corner of our family room and watch TV. Well, watch is the wrong word, the TV was on and I was aware of it but I couldn’t concentrate on anything long enough to get interested in it. That recliner became my home off and on for almost two years.
Each day as my physical health improved I went through the motions of living but without enthusiasm and always with a feeling of impending doom. I attributed some of my mood to being forced to retire from a profession I loved which meant I was no longer able to support us. For the first time since I was ten years old I didn’t have a job and felt too old and useless to get one. I did everything my doctors advised; physical therapy, watched my diet, tried to get exercise, tried to live a normal life but deep down I just didn’t give a damn. I wasn’t suicidal I was just a kind of zombie.
My wife, Robin, was running two of her own businesses at the time and made tremendous sacrifices to help me recover including trying to involve me in her business by giving me simple and easy jobs to do but I wasn’t interested. I owed her my interest and should have helped her because I was capable of doing what she wanted but I preferred feeling sorry for myself while sitting in my dark corner with the flickering images of an unwatched TV set changing the room’s shadows.
While I was being treated for depression, it seemed as though none of the medications really worked very well. Some would give me a lift for a few weeks but almost always would fail and I’d be back in my recliner. I finally got to the point where I believed I was as good as I was going to get. Enter a new therapist.
At my clinic a change in staff resulted in my being assigned a different therapist. At the time I thought nothing of it because I didn’t think there was any hope of ever really feeling good. Wrong! She tried a couple of new medications and then all of a sudden things changed. I felt like a new man, I was my old self…better than my old self, I felt reborn and began living again, doing all the things I used to enjoy but enjoying them even more. It took a little over four years after my transplant to begin living again but it was worth the wait. Incidentally, after trying several drugs and combinations of drugs the one that finally worked was an old one…Remeron.
Post-transplant depression, I understand, can be caused by many factors known and unknown. Two of the most obvious factors are 1) survivors guilt (someone had to die before I could get a transplant), 2) I’m undeserving or, “Why me?” (There are so many younger, sicker people who should have gotten my organ)
Whatever the reason for the depression the fact is that help is available it just may not be immediate. I now know that you cannot give up, you must fight every inch of the way until you get relief. It is not normal to feel down, useless, unimportant and insignificant every waking moment of every day. It just isn’t normal so don’t accept it. Find help. I’m really enjoying life again. You can, too.
Helpful links
Supporting a family member or friend http://www.mayoclinic.com/health/depression/MH00016
Post transplant depression http://surgery.about.com/od/ingandsurgery/a/TransplantCope.htm
All about Depression http://www.allaboutdepression.com/gen_01.html
Consider what I’ve written, discuss it with friends, join discussions on Facebook’s Organ Transplant Initiative and comment in the space provided here. When you have decided what you think is the best solution to the organ shortage contact your elected representative or U.S. Senator and let them know your feelings. Change has to begin somewhere, why not with you?
Bob Aronson of Bob’s Newheart is a 2007 heart transplant recipient, the founder of Facebook’s nearly 3,000 member Organ Transplant Initiative and the author of most of these donation/transplantation blogs.
You may comment in the space provided or email your thoughts to me at bob@baronson.org. And – please spread the word about the immediate need for more organ donors. There is nothing you can do that is of greater importance. If you convince one person to be an organ and tissue donor you may save or positively affect over 60 lives. Some of those lives may be people you know and love.
Please view our new music video “Dawn Anita The Gift of Life” on YouTube https://www.youtube.com/watch?v=eYFFJoHJwHs. This video is free to anyone who wants to use it and no permission is needed.
If you want to spread the word personally about organ donation, we have another PowerPoint slide show for your use free and without permission. Just go to http://www.organti.org and click on “Life Pass It On” on the left side of the screen and then just follow the directions. This is NOT a stand-alone show; it needs a presenter but is professionally produced and factually sound. If you decide to use the show I will send you a free copy of my e-book, “How to Get a Standing “O” that will help you with presentation skills. Just write to bob@baronson.org and usually you will get a copy the same day.
Also…there is more information on this blog site about other donation/transplantation issues. Additionally we would love to have you join our Facebook group, Organ Transplant Initiative The more members we get the greater our clout with decision makers.
En Espanol
Puede comentar en el espacio proporcionado o por correo electrónico sus pensamientos a mí en bob@baronson.org. Y – por favor, difundir la palabra acerca de la necesidad inmediata de más donantes de órganos. No hay nada que puedas hacer lo que es de mayor importancia. Si usted convence a una persona de ser donante de órganos y tejidos puede salvar o afectar positivamente a más de 60 vidas. Algunas de esas vidas pueden ser personas que conoces y amas.
Por favor, consulte nuestro nuevo video musical “Dawn Anita The Gift of Life” en https://www.youtube.com/watch?v=eYFFJoHJwHs YouTube. Este video es libre para cualquier persona que quiera usarlo y no se necesita permiso.
Si quieres correr la voz acerca de la donación de órganos personalmente, tenemos otra presentación de PowerPoint para su uso libre y sin permiso. Sólo tienes que ir a http://www.organti.org y haga clic en “Life Pass It On” en el lado izquierdo de la pantalla y luego sólo tienes que seguir las instrucciones. Esto no es un espectáculo independiente, sino que necesita un presentador pero es profesionalmente producida y sonido hechos. Si usted decide usar el programa le enviaré una copia gratuita de mi libro electrónico, “Cómo obtener un pie” O “que le ayudará con habilidades de presentación. Sólo tiene que escribir a bob@baronson.org y por lo general usted recibirá una copia del mismo día.
Además … hay más información sobre este sitio de blogs sobre otros donación / trasplante temas. Además nos encantaría que te unas a nuestro grupo de Facebook, la Iniciativa de Trasplante de Órganos Cuantos más miembros que obtenemos mayor será nuestra influencia con los tomadores de decisiones.

You must be logged in to post a comment.