Blog Archives
Post Transplant Depression, It’s Common and There’s Help!
By Bob Aronson
 Having suffered from post transplant depression myself, I know of what I speak. It hits you like a sledge hammer and keeps pounding away. The pain isn’t physical, it’s emotional and it can be intense, so intense that some consider taking their own lives. Worst of all, few if any of your family and friends understand and some become impatoemt. dsksdddddddddddddlkkkkkkkkkkkkkksddddddddddddddddddddddddddddddddddddddddddddddddddlddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddccsssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssjnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssss with your continued mood swings. They don’t even have the most basic understanding of the disease. While their intentions are good, their advice usually isn’t. They will say things like, “Buck up, My God your’re alive, you got a new heart and you’re alive.” To that I can only say, “I would be happy to buck up if I could, but I can’t. Noone would choose to live like this You can feel useless, unnecessary, irrelevant and totally without purpose. Some patients even feel suicidal, but it doesn’t have to be that way. There is help.
Having suffered from post transplant depression myself, I know of what I speak. It hits you like a sledge hammer and keeps pounding away. The pain isn’t physical, it’s emotional and it can be intense, so intense that some consider taking their own lives. Worst of all, few if any of your family and friends understand and some become impatoemt. dsksdddddddddddddlkkkkkkkkkkkkkksddddddddddddddddddddddddddddddddddddddddddddddddddlddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddddccsssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssjnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnnssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssssss with your continued mood swings. They don’t even have the most basic understanding of the disease. While their intentions are good, their advice usually isn’t. They will say things like, “Buck up, My God your’re alive, you got a new heart and you’re alive.” To that I can only say, “I would be happy to buck up if I could, but I can’t. Noone would choose to live like this You can feel useless, unnecessary, irrelevant and totally without purpose. Some patients even feel suicidal, but it doesn’t have to be that way. There is help.
If there’s one message you should take away from this blog, it is this. Depression is not your fault, you did not cause it and therefore you alone can not fix it. “Cheer up, look at the bright side,” may sound like good advice but it isn’t because it assumes you decided to feel lousy. Who on earth would choose to be depressed? It is sad, but true that sometimes even the people closest to you don’t understand. They continue to hold on to the belief that you can snap out of it if you really want to. The reality of depression just isn’t that simple. Frankly, it is very, very complex and takes highly skilled and trained professionals to help you find your way back to the sunny side of the street.
Unfortunately if you have had or if you are going to have an organ transplant, chances are good that you might fall victim to post transplant depression. Estimates of how many patients become depressed following an organ transplant range from 10 percent all the way up to 50%, but no matter what the percentage the fact is that some people will have serious emotional struggles following their transplant.
One can easily ask, “Depression? Why on earth would anyone be depressed after their life has been saved by the donor/transplantation process?” Well, there are a number of reasons, chief among them is the haunting feeling that someone had to die in order for you to live. The fact is, the person who died, would have died anyway whether they were an organ donor or not and if they were, someone might gain new life as a result, but that’s logic and logic alone cannot solve the problem and help the patient. Besides, there are other issues that contribute to depression like:
- Living with the psychological highs and lows that are sometimes
 caused by immunosuppressives such as corticosteroids
caused by immunosuppressives such as corticosteroids - The steroids you take can have the effect of a mood amplifier. In the first few weeks, especially, when the doses are highest, the medicine will wind you up and make it hard to sleep. The sudden changes in the family — and in your behavior — can be extreme.
- Managing a complex post-transplant regimen that encompasses: (1) multiple meds and schedules, (2) monitoring vital signs, (3) exercise and dietary requirements, (4) regular medical evaluations and lab tests, and (5) lifestyle restrictions on smoking, alcohol, and other potentially harmful substances
- Major life alterations such as transitioning from being critically ill or dying patients and family caregivers to roles that are more wellness-focused)
- Coping with new and taxing financial and economic issues like the cost of transplant surgery, hospital stays, follow-up care, cost of drugs and health insurance.
To some that list of changes is so overwhelming as to be nearly impossible to manage. Some have been seriously ill for such a very long time and so focused on dying that they cannot adjust to an attitude that centers on life and living. What is even worse is that unless the patient is getting professional psychiatric help he or she may not be able to identify a single stressor that brought on their depressed state.
Simply put, depression is a mood disorder that causes a persistent feeling of sadness and loss of interest in those things that had been of great importance. It affects how you feel, think and behave and can lead to a variety of problems. Day to day activities become ponderous and boring and patients sometimes feel their lives are not worth living.
Depression isn’t just feeling “down” and you can’t just “snap out of it.” It can require long-term treatment with either medication, psychological counseling or a combination of the two. Above all you must know that suffering from depression is not a personal weakness. You didn’t bring it on and will power alone cannot defeat it.
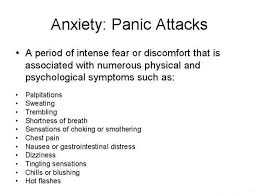
Depression can occur once or several times in a lifetime and according to the Mayo Clinic (http://tinyurl.com/ouory9u) the symptoms can appear all day, every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Changes in appetite — often reduced appetite and weight loss, but increased cravings for food and weight gain in some people
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or blaming yourself for things that aren’t your responsibility
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Other people may feel generally miserable or unhappy without really knowing why. http://tinyurl.com/lgsq8hm
Health Concerns
(Material gathered here comes from several sources primary among them is UNOS (the United Network for Organ Sharing).
What happens after transplantation depends on the organ transplanted and the recipient’s specific medical situation. Most patients recover fully, return to work and resume a normal, active life after receiving a new organ. However, there is a possibility of developing unrelated health problems after transplantation. That’s why it is important to work closely with your doctor concerning your overall wellness, as well as regarding the following health concerns:
Anxiety and Depression
 Patients and their families face a new lifestyle after transplantation that may cause them to feel nervous, stressed or depressed. Because emotional and psychological support is a continuing process, ask your social worker about counseling services that can help you and your family deal with these changes. Professionals can help you work through concerns about your self-image; mood swings; job planning; rehabilitation; family stresses, such as parent-child conflicts, marital conflict or changes in sexual functioning; and financial concerns, such as questions about Medicare, disability or insurance. Any and all of the following can contribute to your depression and/or anxiety.
Patients and their families face a new lifestyle after transplantation that may cause them to feel nervous, stressed or depressed. Because emotional and psychological support is a continuing process, ask your social worker about counseling services that can help you and your family deal with these changes. Professionals can help you work through concerns about your self-image; mood swings; job planning; rehabilitation; family stresses, such as parent-child conflicts, marital conflict or changes in sexual functioning; and financial concerns, such as questions about Medicare, disability or insurance. Any and all of the following can contribute to your depression and/or anxiety.
Diabetes
Some anti-rejection medicines are known to cause high blood sugar. Although it is typically a temporary condition after transplantation, it is more common in patients who have a family history of diabetes and patients who are overweight. It can be controlled by reducing the dose of a patient’s anti-rejection medicines or changing medications all together.
GI Upset
GI (gastrointestinal) or stomach upset is also a common complaint after a transplant. Patients on steroid therapy may be at an increased risk of developing ulcers due to increased hydrochloric acid from the stress of the procedure. Treatment of GI upset may include one or a combination of drugs that reduce acid production. In addition, people with GI upset should take several steps to reduce symptoms, including:
- Reducing the intake of caffeine, alcohol and over-the-counter medications that cause GI upset.
- Eliminating carbonated drinks can help
- And it sometimes helps to take your meds with food to decrease irritation.
Gout
Gout is a painful and potentially disabling form of arthritis. Diagnosing gout can be difficult and treatment plans vary based on a patient’s existing medical problems and medications. Often Gout will show up in the big toe and it is very painful. Sometimes even a bedsheet touching the Gout area will result in extreme pain.
High Cholesterol
Many immunosuppressant drugs can contribute to high cholesterol. This condition therefore affects many transplant recipients. When a patient develops high cholesterol, blood vessels, including the ones attached to the transplanted organ, become clogged, which affects the flow of blood. This slowing of blood flow can affect the success of your transplant and may even lead to heart disease. It is important to talk to your doctor about how to reduce the risk factors of heart disease, including controlling your cholesterol.
Hypertension
Hypertension, or high blood pressure, is common immediately after
transplant. Certain anti-rejection medications, as well as the original disease, all can contribute to hypertension. Treatment of hypertension may include one or a combination of drugs, and often, as anti-rejection medicines are tapered to a maintenance dose, hypertension may decrease. Talk to your doctor about what’s right for you and how to avoid high blood pressure.
Sexual Relations
Sexual concerns after transplantation are commonly experienced, yet seldom discussed or addressed during evaluation. It is therefore very important to talk with your doctor about your sexual history and concerns.
However, sexual function and interest can be related to how well your body has accepted your new organ and how realistic your expectations were for life after your transplant. A counselor can also help a couple understand the difference between pre- and post-transplant problems. Often, support groups can be very helpful in this regard.
Additionally, in sexual relations, as in all issues, recipients must remember that they are immune suppressed and subject to many kinds of infections. In fact, some infections in recently transplanted patients can be potentially life threatening. Consequently, it is important to consider the following points:
- The sharing of saliva during kissing can expose both partners to active diseases, such as colds or other viruses.
- Condoms don’t prevent diseases that are spread by contact between the area surrounding the penis and external genitals.
- The risk of contracting infectious diseases though oral sex is possible, especially if ejaculation occurs or if there are any sores or wounds on either partner.
Shingles
People with weakened immune systems, such as transplant recipients treated with immunosuppressive drugs, risk developing shingles. Shingles is a painful infection of the central nervous system caused by the Varicella virus that causes a blistering rash and severe burning pain, tingling or extreme sensitivity to the skin and is usually limited to one side of the body. The severity and duration of an attack of shingles can be significantly reduced by immediate treatment with antiviral drugs. You should also ask your doctor about getting the Shingles vaccine.
Sometimes our own irresponsible behavior is responsible for feelings of depression or inadequacy. It has been established that noncompliance appears to be relatively common during the first several years after transplantation. That means some patients just don’t take the right amount of medication at the right time, if they take it at all. Furthermore, compliance in most areas of the medical regimen worsens over the first year after the transplant just as it does for most patients who begin new medical therapies. For example:
- Up to 20% of heart transplant recipients and 50% of kidney transplant recipients have been found to be noncompliant with prescribed immunosuppressant medications during a given 12-month period in the early post-transplant years
- 5% to 26% of heart transplant recipients smoke at least once after being transplanted; no study has determined what proportion of these patients become regular smokers.
- 11% to 48% of liver transplant recipients return to some level of alcohol consumption during the first year post-transplantation.
| As a result of noncompliance patients are likely to experience rejection symptoms or actual rejection and, of course when this happens patients experience anxiety and/or depression. http://tinyurl.com/qjlc48n
Treatment options |
 Researchers at Henry Ford Hospital have found that emotional closeness between transplant patients and their caregivers helps reduce depression and anxiety after surgery. While this study was about liver transplant patients, it is likely that the conclusions probably have universal application.
Researchers at Henry Ford Hospital have found that emotional closeness between transplant patients and their caregivers helps reduce depression and anxiety after surgery. While this study was about liver transplant patients, it is likely that the conclusions probably have universal application.
“People with close networks and good support recover faster after liver transplant and have less depression and anxiety at six months after transplant,” says Anne Eshelman, Ph.D., Henry Ford Health System Behavioral Health Services, lead author of the study.
“These findings suggest caregiving relationships as a target for psycho-therapeutic intervention among patients with end-stage liver disease.”
Study results were presented at the International Congress of Behavioral Medicine in Washington D.C., held by the International Society of Behavioral Medicine and the Society of Behavioral Medicine.
The study looked at 74 liver transplant surgery candidates and their primary caregivers. Transplant patients were surveyed before surgery and at a six-month follow-up. Caregivers rated the degree of closeness they felt in their relationship to the patient.
The sample was divided into groups with caregivers reporting maximum closeness or less closeness.
For patients with end-stage liver disease, depression and anxiety improve after liver transplant, but the study found that these changes are not as great for individuals with emotionally distant caregiving relationships.
“If you live with someone who loves you, the quality of care they provide may be much better, they may be more encouraging, you may want to please them and recuperate faster so you can spend quality time with them,” says Dr. Eshelman. “Caregivers who are not close, may provide the basic requirements, but don’t help give someone a reason to live and look to the future.”
The study results also suggested that emotional closeness was critical for affective improvement in men, but less so for women, though interpretation is limited by a small sample size, explained Dr. Eshelman.
“Men who had adequate number of support people, but did not have close support, were still depressed and anxious at follow up, compared to those who had closer support,” says Dr. Eshelman. “Other literature shows that women have wider support, more friends and family they are connected to than men, and if the primary support person is not that close, they probably rely on the other people such as girlfriends.”
The study was funded by Henry Ford Transplant Institute. http://tinyurl.com/q4bwqzs
Treatments for Depression
From Web MD
If you are diagnosed with depression, here’s some good news: Excellent treatment options are available to you.
Many people use a combination of treatments, such as medication and psychotherapy. For depression that doesn’t respond to standard treatment, non-drug approaches can be effective, either alone or used with other treatments.
Learn more here about the most common approaches to treating depression.
Talk Therapy for Depression
Talking with a trained therapist is one of the best treatments. Some people choose to be in therapy for several months to work on a few key issues. Other people find it helpful to continue in therapy for years, gradually working through larger problems. The choice is up to you and your therapist. Here are some common types of therapy:
- Cognitive behavioral therapyhelps you see how behaviors and the way you think about things plays a role in your depression. Your therapist will help you change some of these unhealthy patterns.
- Interpersonal therapyfocuses on your relationships with other people and how they affect you. Your therapist will also help you pinpoint and change unhealthy habits.
- Problem-solving therapyfocuses on the specific problems you face and helps you find solutions.
Medicines for Depression
Medicines are the other key treatment for depression. If one antidepressant doesn’t work well, you might try a similar one or a different kind. Your doctor might also try changing the dose. In some cases, he or she might recommend taking more than one medication for your depression. There are now many different antidepressants that your doctor can choose from. The entire listing can be seen here: http://tinyurl.com/p4yaq4b
doesn’t work well, you might try a similar one or a different kind. Your doctor might also try changing the dose. In some cases, he or she might recommend taking more than one medication for your depression. There are now many different antidepressants that your doctor can choose from. The entire listing can be seen here: http://tinyurl.com/p4yaq4b
Just keep in mind that recovery is a process that may need constant adjustment and takes time.
-0-
Bob Aronson of Bob’s Newheart is a 2007 heart transplant recipient, the founder of Facebook’s over 4,200 member Organ Transplant Initiative (OTI) and the author of most of these donation/transplantation blogs. You may comment in the space provided or email your thoughts to me at bob@baronson.org. And – please spread the word about the immediate need for more organ donors. There is nothing you can do that is of greater importance. If you convince one person to be an organ and tissue donor you may save or positively affect over 60 lives. Some of those lives may be people you know and love. You can register to be a donor at http://www.donatelife.net. It only takes a few minutes. Then, when registered, tell your family about your decision so there is no confusion when the time comes.
Kidney Disease — What You Need To Know
Blog by Bob Aronson
My last blog was about kidney disease and so is this one. “Steering Toward Hope” told about Johnny Racine the Canadian father of 16 year old twin boys and how they turned their 2007 Ford Mustang into an 800 horsepower fire breathing showpiece named “The Kidney Hope Car.” Racine, his boys and the rest of the “Steering” team will travel the width of Canada to promote organ donation and to raise money for kidney research.
This post will take a different but complimentary approach. The law of supply and demand applies to human organs as it does to many other commodities. While we must work harder than ever to increase the supply we must concurrently do everything we can to reduce the demand. It is the only way we will ever arrive at anything even close to resembling a balance of the two.
The following paragraphs will examine kidney disease from several angles — from listening to how patients describe their illness to prevention, treatment and what the future holds.
Before I get into the real life, real people part of this blog, let me first lay out the facts about Chronic Kidney Disease (CKD). It is a major health problem that affects more than 26 million Americans. It is the ninth-leading cause of death in the U.S. While the numbers are different elsewhere every country is having the same experience. Whether you are from Singapore, New Zealand, Canada or Peru you will find that kidney disease is on the rise and there are not enough organs for the number of people who need transplants.
Of the 26 million Americans with kidney disease, about half a million face kidney failure, the condition that requires dialysis. Dialysis, though, is not a cure and in many cases is a stop gap effort while the patient awaits an organ transplant — but transplants are hard to get.
At this writing in November of 2013 there are almost 100,000 people on the list awaiting kidney transplants but 5-6,000 of them die while waiting because the supply of organs not only does not meet demand it is falling farther and farther behind. Unlike other transplants though, one can also get a kidney from a living donor but there aren’t enough of them either in fact the number of living kidney donors has fallen steadily for the past several years, to 13,040 in 2012, despite the growing need. Regardless of the source the average wait time for a Kidney Transplant in the U.S. is 1,121 days.
I’m hoping this blog will help people understand two things. 1) how to prevent kidney disease and 2) what to expect if you get it. But first, I think it is important to discuss what causes CKD.
Causes of Kidney Disease
The two main causes of chronic kidney disease are diabetes and high blood pressure, which are responsible for up to two-thirds of the cases. Diabetes happens when your blood sugar is too high, causing damage to many organs in your body, including the kidneys and heart, as well as blood vessels, nerves and eyes. High blood pressure, or hypertension, occurs when the pressure of your blood against the walls of your blood vessels increases. If uncontrolled, or poorly controlled, high blood pressure can be a leading cause of heart attacks, strokes and chronic kidney disease. Also, chronic kidney disease can cause high blood pressure.
Other conditions that affect the kidneys are:
- Glomerulonephritis, a group of diseases that cause inflammation and damage to the kidney’s filtering units.
- Inherited diseases, such as polycystic kidney disease, which causes large cysts in the kidneys that damage the surrounding tissue
- Repeated urinary infections.
- Pregnancy problems. Sometimes a narrowing of the womb can occur that prevents normal outflow of urine causing it instead to flow back up to the kidney causing infections and kidney damage.
- Lupus and other immune system diseases
- Obstructions caused by kidney stones, tumors or, in men, an enlarged prostate gland.
High risk groups include those with diabetes, hypertension and family history of kidney failure. African Americans, Hispanics, Pacific Islanders, American Indians and senior citizens are at increased risk.
Before we get into the details of kidney disease and what to do if you have it, let us first discuss how to avoid it. While there is no sure fire way to prevent kidney problems there are many very effective steps you can take because lifestyle can be a great contributor to the development of all diseases.
Avoiding Kidney Disease
 The National Kidney Foundation has the following guidelines to reduce the risk of developing kidney disease:
The National Kidney Foundation has the following guidelines to reduce the risk of developing kidney disease:
- Reduce sodium intake: Americans consume too much sodium (salt)
- Limit red meat: Diets high in protein – especially those with animal protein – may harm the kidneys. Red meat is also high in saturated fat.
- Avoid soda: Sugar-sweetened drinks, like sodas, are high in calories and contain no nutritious value. Additionally, colas have phosphorus additives which can damage kidneys.
- Give up processed foods: Potato chips, crackers, cheese spreads, instant potato mix, and deli meats are all examples of processed foods that are high in phosphorus additives and sodium – both of which can have a damaging effect on the kidneys.
- Reduce sugar intake: Consuming too much sugar can result in diabetes or obesity – both linked to kidney disease.
- Sit less and stand more: Recent research has linked sitting for 8 hours or more a day with developing kidney disease.
- Exercise and lose weight: Diabetes is responsible for 44 percent of all new cases of kidney failure. Obesity and Type 2 diabetes are on the rise and can often be treated and reversed.
- Manage high blood pressure: Both considered silent killers, many people don’t realize high blood pressure and kidney disease are linked. Controlling blood pressure levels can prevent kidney damage and failure.
- Avoid long term use of kidney-toxic drugs: Over-the-counter (OTC) pain medications, nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen brand names (Motrin, Advil, and Nuprin).
- Get tested: Ask your doctor for an annual urine test to check for protein in the urine, one of the earliest signs of kidney disease, and a blood test for creatinine
But…there’s a whole lot more to preventing kidney disease. The Correct Diet Can Help Avoid Kidney Disease http://www.medicalnewstoday.com/articles/259203.php (See this link for the full story.)
Bad diet choices and habits like smoking and obesity are linked to  an increased risk for kidney disease, suggests a new study published in the American Journal of Kidney Disease.
an increased risk for kidney disease, suggests a new study published in the American Journal of Kidney Disease.
A group of investigators, led by Alex Chang, MD, of Johns Hopkins University, discovered that people with regular kidneys whose diet quality was bad – high in processed and red meats, sodium, and sugar-sweetened beverages, and low in fruit, nuts, legumes, whole grains, and low-fat dairy – were more likely to develop kidney disease.
Just one percent of people without unhealthy diet or lifestyle choices developed protein in their urine – an early sign of kidney damage. On the other hand, 13% of participants who had at least three unhealthy factors such as obesity, smoking, and poor diet developed protein in their urine.
Obese people, i.e. those with a body mass index (BMI) of at least 30, were twice as likely to develop kidney disease, the authors reported. A poor diet independently influenced risk for chronic kidney disease after adjusting for weight and other influential factors.
In total, those who ended up with kidney disease were more likely…
- to be African American
- to have high blood pressure
- to have diabetes
- to have a family history of kidney disease
- have a higher intake of soft drinks, fast food, and red meat compared to those who did not have kidney disease.
How it Feels to Have Kidney Disease
Now let’s get to the disease itself. The medical profession can describe it in terms no one can understand but I prefer to hear from patients. What does it feel like to have kidney disease, how does your body change? That’s a tough question to answer because so many people have no symptoms or symptoms that are so mild they don’t notice them but we did find some clear, understandable and frightening explanations.
We are going to look at symptoms of kidney failure from two perspectives. First the little tell-tale signs that something might be amiss and secondly the more specific complaints as told by patients. Fist the little signs that indicate you might have kidney disease but don’t diagnose yourself. See your physician. You might have kidney disease if you:
- feel more tired and have less energy
- have trouble concentrating
- have a poor appetite
- have trouble sleeping
- have muscle cramping at night
- have swollen feet and ankles
- have puffiness around your eyes, especially in the morning
- have dry, itchy skin
- Need to urinate more often, especially at night
Now let’s look at more serious conditions. If you are feeling anything like any of the following people you probably should see your doctor as soon as possible.
- “I feel like I have the flu and am cold most of the time and. When I take my temperature, it is normal. I feel sort of dizzy, have a loss of appetite, food doesn’t have any taste, I have shortness of breath, no energy, and am nauseous. It’s pretty miserable.”
- “When I first got sick I really thought it was a normal cold. I had a fever, was sneezing, runny nose etc. Then it got worse to where I was throwing up, had blood coming out in spits, vomit, urine, etc. Then it became really hard to breath and I couldn’t lay down anymore as it would cause me to suffocate. I ended up in the hospital where they told me both my kidneys failed and liquid was pushed up to my lungs which was causing me to suffocate. I don’t want to scare anyone but please learn from my mistake of not going to the hospital for about 3 weeks after I first got the cold like symptoms. Get a check up even if you think it is a cold!”
- “My kidney failure was discovered by accident through routine blood work at the time of my yearly physical. The first red flag was a high potassium level on two different blood draws over a two month period of time. I had observed several symptoms too, The first symptom strangely was an “itchy back,” another one was an “ill feeling” — not being very hungry – sweating — breathlessness — a rapid heart rate — and discomfort (pain) in the location of the left kidney. These “symptoms” did not appear all at once or I would have seen a doctor. I now know that all of these are symptoms of chronic kidney failure. It is vital to be informed and educated.”
- “I was diagnosed about three years ago with stage 3 kidney failure. I had no signs that I was aware of as I also have congestive heart failure. Now, I itch alll over my body, perspire excessively and have extreme pain in my back, neck,shoulders and legs, as well as increased ankle swelling.”
- “I did not realize I had quit urinating until my husband and I went on a long road trip. I didn’t feel the need to stop to urinate at all. I paid no attention at the time but now I remember that I was very nauseous, vomiting, and had horrible leg cramps. On the third day I went to the ER and was admitted to the ICU. After five dialysis treatments I started to recover. I now measure my output just to be sure.”
For the sake of education let’s assume you have been diagnosed with kidney disease. What are your options? There really are only two. 1) you can choose to allow your medical team to treat it with medication and ultimately dialysis. 2) a kidney transplant but you must qualify and only a medical team at a transplant center can determine if you are a candidate for a transplant.
If Dialysis is Ordered
Chronic kidney disease continually gets worse and eventually leads to end-stage renal disease, also known as kidney failure.
\Your doctor might recommend you begin dialysis treatments once you reach the point where you have only 10 to 15 percent of kidney function left.
With kidney failure, the toxins and excess fluid that your kidneys should be releasing begin to build up in your body. People suffering from kidney failure begin dialysis to help their bodies remove these wastes, salts and fluid.
Two kinds of Dialysis
- Hemodialysis and
- Peritoneal dialysis.
Hemodialysis is typically performed at dialysis centers or hospitals but some clinics offer smaller devices for home use.
Hemodialysis, patients generally have an access point in their arm to which the dialysis machine is connected. On average It takes aobut four hours for the blood that is drawn from your body to be cleansed and returned.
Peritoneal dialysis is more likely to be done at home after you have a catheter placed in your stomach (a minor surgery).
There are two kinds of Peritoneal dialysis, 1) continuous ambulatory and 2) continuous cycling
Continuous cycling peritoneal dialysis is usually done at night. Before retiring you attach the dialysis machine tube to your catheter which pumps a solution into your stomach. It stays there for a few hours so your stomach can act as a filter allowing waste and other fluids to pass through it into the solution.
Continuous ambulatory peritoneal dialysis is much different because you don’t need a machine. You simply run dialysis solution into your abdomen through the catheter and after 4k to 6 hours drain it into a bag. A physician can tell you how often during the day you need to do this
Risk Factors
There are several. They include anemia, bone disease, high blood pressure and depression. Some patients on hemodialysis might have also have problems with low blood pressure.
Patients undergoing peritoneal dialysis are at risk of developing peritonitis which is an infection in the stomach lining. Your doctor will likely prescribe antibiotics to treat the problem.
Got questions? Many answers can be found here.
http://www.nwkidney.org/dialysis/startingOut/basic/faqs.html
A Kidney Transplant
If it has been determined that a Kidney transplant is your only option this information may prove to be invaluable.
KidneyBuzz.com encourages patients to stay as healthy as possible by managing stress, eating well, and staying active. It is important for patients to remain as well as possible during this time, so they are ready for kidney transplant surgery as soon as a donor organ becomes available. For patients who have a living organ donor, scheduling transplant surgery can take into account the health status of the recipient as well as other factors.
Manage your stress. Many patients constantly worry about their treatments, blood work results, future surgeries, etc. Education and support groups both online such as KidneyBuzz.com, and offline provide patients with tools and support to manage their stress and cope with the challenges associated with their condition. Recommended Reading: Will You be Ready when Your Time Comes for a Kidney Transplant? (this link and links below from KidneyBuzz)
There are other strategies that you can employ to expedite obtaining a Kidney Transplant including listing at more than one transplant center (Multi-Listing). Research has consistently shown that patients who are strategically Multiple Listed will greatly increase their chances of receiving a Kidney Transplant faster. Nevertheless, only a mere 4.7% of individuals with CKD utilize the Multiple Listing technique.
KidneyBuzz Recommended Reading: “Ins-and -Outs” of Increasing your Chances of Getting a Kidney Faster
There are also website resources available that assist people with CKD to find Kidney Transplant Centers with the lowest average wait times that are the closest to where they live. These free user friendly website tools can be particularly helpful to people who are on a Kidney Transplant Waiting List in a high wait time area because it can significantly increase their access to Kidney Transplant Centers options with far lower wait times. You can email KidneyBuzz.com at contact@kidneybuzz.com for more information and direct links to discussed sites.
Once you have determined the treatment track you will take the next  big question most people have is, “How do I pay for the it?” Well, if you have regular health insurance that might cover it. If not the National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) http://kidney.niddk.nih.gov/kudiseases/pubs/financialhelp/ offer this information”
big question most people have is, “How do I pay for the it?” Well, if you have regular health insurance that might cover it. If not the National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) http://kidney.niddk.nih.gov/kudiseases/pubs/financialhelp/ offer this information”
In 1972, Congress passed legislation making people of any age with permanent kidney failure eligible for Medicare, a program that helps people age 65 or older and people with disabilities pay for medical care, usually up to 80 percent. The remaining 20 percent can still pose a significant financial burden on patients. Fortunately, other public and private resources can help. Anyone with permanent kidney failure who does not have adequate insurance coverage should seek the help of a certified or licensed social worker. Every dialysis and transplant center has a social worker who can help people with kidney failure locate and apply for financial assistance. Social workers who specialize in helping kidney patients are called nephrology social workers.
Patients can also enlist the assistance of the State Health Insurance Assistance Program (SHIP). The SHIP is a national program that provides free counseling and assistance to Medicare beneficiaries on a wide range of Medicare and supplemental insurance matters. Patients can find a state program by visiting shipnpr.shiptalk.org/shipprofile.aspx ![]() .
.
To qualify for Medicare on the basis of kidney failure, a person must require regular dialysis or have had a Medicare-covered kidney transplant and must have paid into Social Security through an employer-or be the child or spouse of someone who has or have worked under the Railroad Retirement Board, or as a government employee-or be the child or spouse of someone who has or already be receiving Social Security, Railroad Retirement, or Office of Personnel Management benefits.
The Original Medicare Plan has two parts: Part A is hospital insurance, and Part B is medical insurance. Part B covers most outpatient services, including kidney dialysis, doctors’ services, outpatient hospital services, and many other health services and supplies. While Part A has no premiums, most Part B services require premiums, deductibles, and coinsurance.
Some people who are not eligible for Medicare because they have not worked at a job that pays into Social Security may still be eligible to buy Medicare coverage by paying premiums for Part A.
For more information check with the NKUDIC (link posted above)
 Jay Robare is a friend and a member of my Facebook group Organ Transplant Initiative. He is the talent behind the design of the OTI logo. Jay is legally blind and has been on the kidney transplant list for about four years. He wrote this about two years ago when he lived in Fort Lauderdale, Florida. He is now a resident of Philadelphia, Pennsylvania. Here’s Jay’s story….he’s still waiting.
Jay Robare is a friend and a member of my Facebook group Organ Transplant Initiative. He is the talent behind the design of the OTI logo. Jay is legally blind and has been on the kidney transplant list for about four years. He wrote this about two years ago when he lived in Fort Lauderdale, Florida. He is now a resident of Philadelphia, Pennsylvania. Here’s Jay’s story….he’s still waiting.
The Jay Robare Story
Waiting for a Kidney
By the time that I was approved for Medicare, I had gone through all my savings and my limited insurance coverage. I had to quit working because my endurance was gone and because I was not working, I could not afford my apartment anymore and I had to start living with others that helped me out. I lost all my furniture and most of my art equipment.
I finally got disability insurance and was qualified for Medicare but not Medicaid since I was making too much money from disability; I got enough to pay rent and had some money for paper products, which costs a lot. I have to dry my hands on paper towels to stay sterile.
I was blessed with $200 in food stamps last year but that has been decreased too; I am out of food by the third week of the month. I keep asking for rides to the various food banks but people are too busy. I am not the only one going through this; most people just can’t understand the magnitude of what we are going through in our lives and in our bodies. I know everyone is having problems for I hear that all the time but when I got sick and started working to get on the waiting list, all my doctors and nurses treated me like I was given a special gift which it is…the gift of life but many people would rather worry about their financial or relationship problem that they will outlive. We won’t outlive our problems, they are literally killing us.
****Editors note. (When Jay lived in fort Lauderdale he was on Peritoneal Dialyisis…he is no longer but I included it because patient should know about it.)
I didn’t even talk about having to do dialysis every night. The type of dialysis that I do is called Peritoneal Dialysis where I store 2,500 milliliters of sugar saline solution for 2 and a half hour cycles 4 times which is all carbohydrates. I have gained 30 Lbs and I look very well fed; my fried Dirk said I looked like I had a beer belly…my last beer was a Heineken last Christmas. One nice thing about PD instead of hemo dialysis is that I have no liquid restraints. On hemo, I could only have 60 Oz a day or I would risk cramping and THAT was a bitch. Cramps formed in muscles that I thought I never had and the pain was so bad it made me yell out for Jesus…made my tech laugh at me.
Speaking of techs, I had clowns that would not listen to me and do the treatment their own way ending up hurting me. For you on Hemo, THIS IS YOUR TREATMENT AND YOUR BODY, don’t take any crap from these people; make sure that your nurse knows and the director knows that you do not want this person touching you again. Another thing that I like about PD is that it is robbing my body of potassium and this lets me eat things that hemo would never let me eat like bananas, mashed potatoes, spinach, hummus, vegetables and fruits. I do have to take something called a binder every time that I eat something. This medicine absorbs all the phosphorus in the food. The binder can be nasty at times, it is very dry and tastes like I am eating chalk. The chalk does a good job but sometimes it is difficult to take. The meds are a chewable but I think they are coming out with a powder soon.
Another med that I have to take because of PD and a bad parathyroid, caused by ESKD is a drug called Zemplar and Sensipar. Both keep my calcium land my PTH levels down. The only problem is that Sensipar has made me nauseous for the last 4 years; I have been throwing up every time I took this drug for 7-8 months. I guess my body has had enough. The doctors, dietitians and I have been playing games for years. I have finally decided to have a perthyroidectomy. After this surgery, I will need to start taking calcium supplements, including eating more pizza and lasagna…LOL I
I get extremely tired sometimes during the day from either walking to the bus stop and going to Publix to get some noodles or walking from the bus stop to my Davita dialysis clinic to get labs done every Monday or Tuesday; I need to send a vile of blood to my transplant hospital every week so they can keep an eye on my health and changes in my DNA.
*** Editors Note (Jay is now living in Philadelphia and is on hemodialysis which limits his liquid intake. He is desperately trying to find a living donor. This journey has been very hard on Jay yet somehow he manages to keep his spirits up.
The Kidney Transplant
 Everyone has two kidneys, each the size of a fist and they have a very important job to do. They filter waste and remove extra water from your blood to make urine. But…there’s more. Your kidneys also control your blood pressure and make hormones that your body needs to stay healthy.
Everyone has two kidneys, each the size of a fist and they have a very important job to do. They filter waste and remove extra water from your blood to make urine. But…there’s more. Your kidneys also control your blood pressure and make hormones that your body needs to stay healthy.
During a kidney transplant
Kidney transplants are performed with general anesthesia, so you’re not aware during the procedure. The surgical team monitors your heart rate, blood pressure and blood oxygen level throughout the procedure.
During the surgery:
- The surgeon makes an incision and places the new kidn
 ey in your lower abdomen. Unless your own kidneys are causing complications such as high blood pressure or infection, they are left in place.
ey in your lower abdomen. Unless your own kidneys are causing complications such as high blood pressure or infection, they are left in place. - The blood vessels of the new kidney are attached to blood vessels in the lower part of your abdomen, just above one of your legs.
- The new kidney’s ureter — the tube that links the kidney to the bladder — is connected to your bladder.
Kidney transplant surgery usually lasts about three to four hours.
After a kidney transplant
After your kidney transplant, you can expect to:
- Spend several days to a week in the hospital. Doctors and nurses monitor your condition in the hospital’s transplant recovery area to watch for signs of complications. Your new kidney will make urine like your own kidneys did when they were healthy. Often this starts immediately. In other cases it takes several days. Expect soreness or pain around the incision site while you’re healing.
- Have frequent checkups as you continue recovering. After you leave the hospital, close monitoring is necessary for a few weeks. Your transplant team will develop a checkup schedule for you. During this time, if you live in another town, you may need to make arrangements to stay close to the transplant center.
- Take medications the rest of your life. You’ll take a number of medications after your kidney transplant. Drugs called immunosuppressants help keep your immune system from attacking your new kidney. Additional drugs help reduce the risk of other complications, such as infection, after your transplant.]
http://www.mayoclinic.org/kidney-transplant/kidney-transplant-procedure.html
The Future
What does the future hold? It is easy to speculate about what the future holds and absolutely impossible to be accurate. We just don’t know. Is there promise? Yes! There are many promising developments taking place in laboratories around the world every day. We won’t go in to all of them because if history is any indicator most of those experiments will fail. There are some, though, that hold some promise at least for now…like this one.
Intravenous Kidney Cell Transplant Experiments Raise Hope for Future Human Kidney Failure Treatments
May 31, 2012 — Indiana University School of Medicine scientists have successfully transplanted primary kidney cells intravenously to treat renal failure in rats, pointing the way to a possible future alternative to kidney transplants and expensive dialysis treatments in humans.
The researchers, Katherine J. Kelly, M.D., associate professor of medicine, and Jesus Dominguez, M.D., professor of medicine, genetically modified the cells in the laboratory to produce a protein — called SAA — that plays an important role in renal cell growth, embryonic kidney development and kidney regeneration after an injury. Modified cells found their way to the appropriate locations of the damaged kidneys, resulting in regeneration of tissue and improved function in the kidney.
The researchers’ work has been accepted for publication in the American Journal of Physiology — Renal Physiology, which published an advance online version of the paper on May 16. You can read more here http://www.sciencedaily.com/releases/2012/05/120531135645.htm
-0-
 Bob Aronson is a heart transplant recipient. He got his new heart on August 21,2007 at the Mayo Clinic in Jacksonville, Florida where he now lives with wife Robin and their two dogs Reilly, a soft coated Wheaten, and Ziggy a Mini Schnauzer.
Bob Aronson is a heart transplant recipient. He got his new heart on August 21,2007 at the Mayo Clinic in Jacksonville, Florida where he now lives with wife Robin and their two dogs Reilly, a soft coated Wheaten, and Ziggy a Mini Schnauzer.
For some 25 years before his transplant Bob was an international communications consultant and owner of the Aronson Partnership which became the Aronson Communications Group after the surgery. Today he is semi retired and also assists his artist wife Robin with her Jinglers Jewelry art show business.
Prior to starting his consulting firm in the 1980s he served as the Communications Director for a Minnesota Governor; was the first Anchor of Morning Edition on the Minnesota Public Radio Network; worked as a journalist at several Midwest broadcast facilities and from 1965 to 1974 was one of the first radio talk show hosts in the country.
Aronson founded Bob’s Newheart and Facebook’s Organ Transplant Initiative (OTI) on November 3, 2007. OTI is a 3,000 member transplant patient, recipient, caregiver and donor/donor family support and education group.
Readers are welcome to Join OTI with the only requirement being that you support our mission which can be found in the “About” section of OTI. We seek to grow our membership because by so doing will have more influence with decision makers as we pursue those issues which would most benefit our members.
Please view our music video “Dawn Anita The Gift of Life” on YouTube https://www.youtube.com/watch?v=eYFFJoHJwHs. This video is free to anyone who wants to use it and no permission is needed.
Thank you for reading our Bob’s Newheart blogs and please leave a comment or contact Bob directly at bob@baronson.org. We intend to continue to expand the number of issues we cover and the availability of information to the public. You’ll find scores of other posts on Bob’s Newheart, just check the index for topics, click and read.
If you are an organ donor we thank you. If not you can become one by going to www.donatelife.net it only takes a few minutes. Then, tell your family what you have done so there is no confusion later.
The Answers to Most Post Transplant Questions
If you are a regular Bob’s NewHeart reader you know I have posted hundreds of articles on donation/transplantation issues and you might think that by now I, myself, would be a pretty good source of information. Well, whenever I let myself think that, even for a second, I stumble across something new that reminds me that I am only a reporter, not a medical expert.
Your Questions Answered
Some of the most common questions I hear from readers include, ”What can I expect after my transplant? What will life be like? Will I be able to resume a normal life right away? Will there be complications? Well, it’s hard to find the answers to all those questions in one place but today’s post comes about as close as any I’ve seen.
This is a great resource for both pre and post organ/tissue transplant patients. Please read it and pass it on. It is a reprint from the American Society of Transplantation (AST) publication “Healthy Transplant.” Let them know you appreciate their efforts on your behalf.
Some of the graphs and charts may be too small for you to read but if you click on the link you can enlarge and study them.
http://www.healthytransplant.com/health_maintenance/health_after_transplantation.aspxHealth After Transplantation
KEEPING A HEALTHY OUTLOOK ON LIFE
After an organ transplant, there is hope for the future. However, there are a number of health concerns that you will face. For example, there is the chance that your new organ will not always function as well as it should. Transplant recipients also have a higher risk of developing certain conditions such as high blood pressure, high blood lipid levels, diabetes, kidney problems, liver problems, and bone disease. Infection and cancer are also conditions you need to keep in mind.
Some conditions can affect any transplant recipient and some conditions are specific to the type of organ transplanted.
|
|
|
|
|
|

CARING FOR YOUR NEW ORGAN
Lab Tests for Measuring Organ Function
It is important to keep all of your scheduled checkups and lab appointments for monitoring organ function. Testing allows your transplant team to monitor the status of your transplant, detect rejection early, and start effective therapy right away.
Common tests for checking organ function are listed below:
|
|
OTHER HEALTH ISSUES
Anti-rejection medications increase your risk of developing certain conditions such as infection and cancer. Other side effects of some anti-rejection medications include high blood pressure, diabetes, high blood lipids, kidney disease, heart attack, stroke, and bone disease. Knowing the risks and taking steps now to prevent them is a good way to keep you and your new organ healthy.
HIGH BLOOD PRESSURE
High blood pressure (hypertension) is a common complication in patients who receive a transplant. High blood pressure can damage the arteries and the heart, increasing the risk of a stroke, a heart attack, kidney problems, or heart failure.
For many patients, the cause of hypertension is not known. However, people with kidney disease, diabetes, or high blood pressure before the transplant are at higher risk of high blood pressure after the transplant. Other factors that contribute to high blood pressure after a transplant include a diet high in salt, clogged arteries, high blood lipid levels, smoking, obesity, and some anti-rejection medications such as cyclosporine, tacrolimus, and steroids (prednisone).
Recommended Blood Pressure Levels
People with a blood pressure of 140/90 mm Hg or higher are considered hypertensive. While most transplant recipients should have a blood pressure of 130/80 mm Hg, the ideal blood pressure can vary from person to person. The American Heart Association (AHA) guidelines for the target blood pressure in the general population can also be used as guidelines for organ transplant recipients. Normal blood pressure values for children are based on age, sex and height and in general are much lower than in adults.
|
Classification |
Systolic Pressure (mm Hg) |
Diastolic Pressure (mm Hg) |
|
Normal |
Less than 120 |
Less than 80 |
|
Prehypertension |
120-139 |
80-89 |
|
Stage 1 hypertension |
140-159 |
90-99 |
|
Stage 2 hypertension |
160 or higher |
100 or higher |
High blood pressure usually does not cause any symptoms so it is important to have your blood pressure checked by your transplant team at regular follow-up exams. Your transplant team may also want you to monitor your blood pressure closely while at home.
Reducing High Blood Pressure
Making some lifestyle changes can lower your blood pressure and prevent hypertension
Figure. Lifestyle changes for healthier living.

Sometimes hypertension can be controlled with lifestyle changes such as diet and exercise, but most patients also require medication.
There are a variety of medications for treating and controlling high blood pressure
Figure. Blood pressure medications

The most commonly prescribed medications include ACE inhibitors, ARBs, calcium channel blockers, beta-blockers, and diuretics. Some of these medications may have interactions with certain anti-rejection medications.
HIGH BLOOD LIPIDS
While lipids (cholesterol and related compounds) in your blood are necessary for good health, too high levels of some lipids can increase your risk of cardiovascular disease, a leading cause of death among transplant recipients. Most transplant recipients develop high blood lipids. Kidney, heart, and liver transplant patients usually display similar elevations in total cholesterol (TC) and low-density lipoprotein (LDL) cholesterol (“bad cholesterol”).
Eating the wrong foods, lack of exercise, and being overweight can increase your risk of developing high levels of LDL cholesterol (“bad cholesterol”), high levels of triglycerides, and low levels of HDL cholesterol (“good cholesterol”). Transplant recipients who are obese, smoke cigarettes, or have high blood pressure are more likely to have high cholesterol. Steroids and some of the other anti-rejection medications, such as cyclosporine, sirolimus, and tacrolimus, can also cause high blood lipid levels.
Recommended Blood Lipid Levels
Be sure to ask your doctor what your cholesterol levels should be. In some instances, transplant recipients can follow target levels of blood lipids recommended in the National Cholesterol Education Program (NCEP) guidelines.
|
Lipid |
Low |
Optimal |
High |
|
LDL Cholesterol |
|
< 100 mg/dL |
160-189 mg/dL |
|
HDL Cholesterol |
< 40 mg/dL |
|
60 mg/dL |
|
Total Cholesterol |
|
|
240 mg/dL |
Reducing High Blood Lipid Levels
Making healthy lifestyle changes can lower your chances of developing heart disease. You can help lower your blood lipid levels with a proper diet and regular exercise. A diet low in cholesterol and saturated fats may also help reduce your risk of coronary artery disease. In addition to making healthy changes to your diet, exercising for a minimum of 20 to 30 minutes 3 to 4 times a week can also reduce your lipid levels and lower your risk of heart attack or stroke. If you smoke, it is important that you STOP!
If adjustment of your anti-rejection drugs, diet, and exercise are not successful in reducing lipid levels, your doctor may want you to take cholesterol-lowering medications. There are several medications that work to lower blood lipids. The most commonly prescribed medications are called statins, which include atorvastatin (Lipitor®), simvastatin (Zocor®), pravastatin (Pravachol®), fluvastatin (Lescol®), rosuvastatin (Crestor®), and lovastatin (Mevacor®).
If your doctor prescribes a statin, you will need to be monitored for side effects because the risk of side effects is greater when taken with anti-rejection medications. You will also need blood tests to monitor liver and muscle function. Other types of medication that your transplant team might prescribe to treat high blood lipids include bile acid sequestrants, nicotinic acid, fibric acids, and cholesterol absorption inhibitors.
DIABETES
High blood glucose can cause many health problems, including diabetes, heart disease, kidney injury, nerve damage, and eye problems.
Post-transplant diabetes (PTDM) is more common in transplant recipients who have a family history of diabetes as well as those who are overweight, are taking steroids, or have hepatitis C. Diabetes after a transplant is also more common among African Americans and some other ethnic groups such as Native Americans. Other risk factors for PTDM include older age of the recipient.
Controlling Blood Sugar Levels
Most transplant recipients with diabetes can follow the American Diabetes Association (ADA) guidelines. Patients with PTDM should establish a healthy (weight-reducing, if necessary) diet with a structured exercise program. A healthy diet is needed to prevent diabetes or to help control your glucose if diabetes does occur. For all transplant recipients, it is best to eat a healthy diet and exercise regularly to avoid weight gain and reduce the risk of developing high blood glucose or diabetes.
Your transplant coordinator or dietician can help determine your recommended daily calorie intake. Limiting the amount of fats and sugar in your diet can also help to maintain a healthy level of blood glucose.
Treatment Options for Controlling Diabetes
There are several types of medications available for patients with diabetes. Depending on the level of glucose in your blood, treatment with oral hypoglycemic drugs and/or insulin may be indicated. For many transplant recipients, insulin injections or an insulin pump is an option for controlling blood sugar. Or, you may be given an oral medication to control blood glucose levels. Your transplant team will determine which medication is right for you.
KIDNEY DISEASE
Kidney function is often decreased in transplant recipients. This may be caused by a pre-existing condition such as diabetes, high blood pressure, or injury to the kidney before a transplant. Or it may be caused by medications used to prevent rejection after a transplant.
The best way to help prevent kidney disease is to keep your blood pressure and blood glucose under control and to maintain a healthy weight. In addition, regular checkups with blood and urine tests will give your doctor important information for detecting early changes in kidney function and allowing appropriate steps to be taken.
BLOOD VESSELS DISEASE
Transplant recipients have a higher risk of developing blood vessel disease. Some anti-rejection medications increase the risk of high lipid levels, which can clog arteries and restrict the flow of blood to the heart and brain. Deposits — called atherosclerotic plaque — can completely or partially block blood vessels resulting in a myocardial infarction (heart attack) or acute coronary syndromes.
Likewise, a stroke can occur if an artery that supplies blood to the brain becomes blocked. Partial blockage may temporarily reduce the blood supply to the brain. A complete loss of blood supply to the brain results in a stroke.
BONE DISEASE
Bone disease is a problem for many organ transplant recipients. Organ failure before your transplant may cause bones to become thin and brittle (osteoporosis). Other causes of osteoporosis include use of some anti-rejection drugs (corticosteroids), overactive parathyroid gland, cigarette smoking, and not enough calcium in your diet.
Preventing Bone Disease
There are some basic things you can do to help prevent or treat bone disease.
- Exercise regularly, including weight lifting or strength training — be sure to discuss weight limits with your transplant team before beginning an exercise program
- Eat foods that are high in calcium, including low-fat yogurt, cheese, and milk
- Choose foods and juices with calcium added
- Get plenty of dietary protein (unless restricted by your doctor)
- Take calcium supplements if directed by your doctor
- Take vitamin D only as directed by your doctor
- Stop smoking
Your doctor or transplant dietician will tell you if you need to take calcium or vitamin D supplements. Your doctor may also want you to take medications that prevent bone thinning, including bisphosphonates such as alendronate (Fosamax®), etidronate (Didrocal®), and risedronate (Actonel®) or calcitonin.
STAYING FIT
Diet – Things are shaping up
The recommended diet for transplant patients consists of 30% fats, 50% carbohydrates and 20% protein.
Figure. Recommended composition of diet for transplant recipients

Your transplant dietician will give you specific instructions about your recommended daily allowance of specific nutrients. Some tips for following a healthy diet include:
- Eat high-fiber foods such as raw fruits and vegetables
- Increase your calcium intake by eating low-fat dairy products and green leafy vegetables or by taking calcium supplements (if directed by your doctor)
- Eat less salt, processed foods, and snacks
- Use herbs and spices to add flavor instead of salt
- Drink plenty of water (unless you are told to limit fluids)
- Eat as little fat and oil as possible
- Eat high-protein foods such as lean meat, chicken (without the skin), fish, eggs, nuts (unsalted), and beans
- Select healthier condiments such as mustard, low-fat mayonnaise, and low-fat salad dressing
- Instead of frying, try baking, broiling, grilling, boiling, or steaming foods
- Instead of using oil to cook, use nonstick, fat-free spray
Exercise
Exercise is a great way to help increase your energy and strength after a transplant. A regular exercise routine will also help you maintain your ideal weight, prevent high blood pressure and high lipid levels, and keep your bones strong. It also helps relieve stress and overcome feelings of depression.
Soon after your transplant, you’ll want to start slow with a low-impact activity such as walking. With time, you can increase your workout with more demanding activities such as bicycling, jogging, swimming, or whatever exercise you enjoy. Training with dumbbells, cuff weights, or weights will increase strength and help prevent bone loss, but check with your transplant team first to determine how much weight is safe for you to lift. Stretching exercises are also important for muscle tone and flexibility. Be sure to check with your doctor before beginning or changing your exercise routine.
STOP Smoking
Smoking also contributes to already high risk of cardiovascular, particularly in patients with diabetes and may be detrimental to kidney function. Transplant recipients who smoke should to STOP smoking as soon as possible.
Dental Care
Routine dental care is important both before and following transplantation as oral infections can cause significant medical problems and even death. According to the American Heart Association (AHA), pre-treatment with antibiotics is not needed for routine dental care unless the patient has an underlying heart condition that increases the risk of developing a heart infection. These include patients with heart transplants with graft valvulopathy (or a previous history of endocarditis, prosthetic valves, and certain forms of congenital heart diseases.)
Gingival overgrowth (hypertrophy) is a dental issue that can arise in transplant patients especially those using cyclosporine. This occurrence of gingival overgrowth can be reduced by practicing good oral hygiene.
ROUTINE FOLLOW-UP EXAMS
All people should have regular exams to help prevent illness.
As we get older, there are some specific tests that should be done on a regular basis
Figure. Recommended tests by patient age

Self-Monitoring
In addition to the tests that your transplant team will perform at regular follow-up visits, you will need to do some self-testing at home. Here are some things you will need to monitor:
- Weight – Weigh yourself at the same time each day, preferably in the morning. If you gain 2 pounds in a day or more than 5 pounds total, call your transplant team.
- Temperature – You should take your temperature daily, especially when you feel like you have a fever. Call your transplant team if your temperature is too high.
- Blood pressure – Check your blood pressure as often as your transplant team recommends.
- Pulse – You should check your pulse daily. A normal heart rate when not exercising should be 60 to 100 beats per minute. (If you have had a heart transplant, your resting heart rate may be as high as 110 to 120 beats per minute.)
- Blood sugar – If you have high blood sugar or diabetes, you will need to monitor your blood sugar using a glucometer.
Do not take any pain medication (for example, Tylenol®, Motrin®, or Advil®), cold remedy, antacid, herbal medication, or any over-the-counter medication unless your transplant team tells you to.
PREGNANCY: BENEFITS AND RISKS
For female transplant recipients of child-bearing age, fertility is usually restored immediately after a transplant.
There have been thousands of births among women with transplanted organs.
Figure. Number of pregnancies in the US reported in organ transplant recipients

Although pregnancy is now an expected part of the benefits afforded to women by organ transplantation, there are also a number of considerations.
Getting pregnant is generally not recommended within the first year after a transplant because the doses of anti-rejection medications are highest; there is a greater risk of rejection; and many other medications are prescribed that are toxic to the developing fetus. Female transplant recipients of child-bearing age should continue using birth control until the doctor says that it is okay to get pregnant.
Male transplant recipients may also be concerned about their ability to have children. Men may have fertility problems related to some transplant medications, but many men have been able to father healthy children after a transplant.
If you are interested in, or thinking about, becoming pregnant you must talk to your transplant team first. Pregnancy should be planned when organ function and anti-rejection therapy are stable and there are no signs of rejection, high blood pressure, or infection.
High Risk Pregnancy
According to National Transplantation Pregnancy Registry (NTPR) over 70% of births to female transplant recipients are live births and most have favorable outcomes for child and mother. Although this success is encouraging, these pregnancies are still considered high risk. There are risks of complications during pregnancy for the transplant recipient as well as risk of infection and exposure to anti-rejection drugs for the fetus.
For example, there is a greater risk of high blood pressure during pregnancy in the woman who has received a transplant. The risk of infection is higher for all transplant recipients, and urinary tract infections are the most common infections during pregnancy. Other infections that may cause concern during pregnancy include herpes, hepatitis, toxoplasmosis, and cytomegalovirus. Other risks include preeclampsia and preterm delivery. The fetus is also at risk for infections such as cytomegalovirus and herpes simplex virus related to the suppression of the mother’s immune system by anti-rejection drugs.
A common question is whether the baby born to a woman with a transplanted organ will be normal. We know that some babies are born premature to mothers with transplants and that they have low birth weights. It is not known whether there are long-term effects on the baby’s development.
You should inform your baby’s pediatrician that your baby was exposed to anti-rejection drugs in the womb. There is a higher risk of birth defects with some anti-rejection drugs especially mycophenolate mofetil and azathioprine. The levels of anti-rejection drugs in the mother’s blood must be monitored closely. Monitoring of blood levels is particularly important in the third trimester, when fetal metabolism may increase the clearance of anti-rejection drugs from the blood. Ask your transplant team whether or not you should breast-feed. It is not known whether breast-feeding while on certain anti-rejection medications can harm the baby.
A major concern for transplant recipients is whether pregnancy will lead to organ rejection or decreased function of the transplanted organ. In general, pregnancy does not affect organ function or patient survival as long your organ is working very well. But, it is very important to discuss with your transplant team whether or not a pregnancy will be too risky. Because pregnancy is considered high risk for transplant recipients, your transplant team may recommend and work with an obstetrician who specializes in high-risk pregnancies.
References
Armenti Clin Transpl. 2006:57-70
Cohen. Am J Kidney Dis. 2001;38:S10-24
Eyre. Circulation 2004;109:3244-55
Feurer. Minerva Chir. 2002;57:257-71
Grundy. Circulation 2004;110:227-39
McCashland. Liver Transpl. 2001;7:S2-12
McGuire. Am J Transplant. 2009;9:1988-2003
McKay. Am J Transpl 2005; 5:1592–1599
McKay. Clin J Am Soc Nephrol 2008;3: S117–S125
McKay. N Engl J Med 2006;354;12
Padiyar. Prim Care. 2008;35:433-50
Steinman. Transplantation. 2001;71:1189-204
Ward. J Ren Nutr. 2009;19:111-22
Wilson. J Am Dent Assoc 2007; 138: 739–745, 747–760
Bob Aronson of Bob’s Newheart is a 2007 heart transplant recipient, the founder of Facebook’s nearly 3,000 member Organ Transplant Initiative and the author of most of these donation/transplantation blogs.
You may comment in the space provided or email your thoughts to me at bob@baronson.org. And – please spread the word about the immediate need for more organ donors. There is nothing you can do that is of greater importance. If you convince one person to be an organ and tissue donor you may save or positively affect over 60 lives. Some of those lives may be people you know and love.
Please view our new music video “Dawn Anita The Gift of Life” on YouTube https://www.youtube.com/watch?v=eYFFJoHJwHs. This video is free to anyone who wants to use it and no permission is needed.
If you want to spread the word personally about organ donation, we have another PowerPoint slide show for your use free and without permission. Just go to http://www.organti.org and click on “Life Pass It On” on the left side of the screen and then just follow the directions. This is NOT a stand-alone show; it needs a presenter but is professionally produced and factually sound. If you decide to use the show I will send you a free copy of my e-book, “How to Get a Standing “O” that will help you with presentation skills. Just write to bob@baronson.org and usually you will get a copy the same day.
Also…there is more information on this blog site about other donation/transplantation issues. Additionally we would love to have you join our Facebook group, Organ Transplant Initiative The more members we get the greater our clout with decision makers.
En Espanol
Puede comentar en el espacio proporcionado o por correo electrónico sus pensamientos a mí en bob@baronson.org. Y – por favor, difundir la palabra acerca de la necesidad inmediata de más donantes de órganos. No hay nada que puedas hacer lo que es de mayor importancia. Si usted convence a una persona de ser donante de órganos y tejidos puede salvar o afectar positivamente a más de 60 vidas. Algunas de esas vidas pueden ser personas que conoces y amas.
Por favor, consulte nuestro nuevo video musical “Dawn Anita The Gift of Life” en https://www.youtube.com/watch?v=eYFFJoHJwHs YouTube. Este video es libre para cualquier persona que quiera usarlo y no se necesita permiso.
Si quieres correr la voz acerca de la donación de órganos personalmente, tenemos otra presentación de PowerPoint para su uso libre y sin permiso. Sólo tienes que ir a http://www.organti.org y haga clic en “Life Pass It On” en el lado izquierdo de la pantalla y luego sólo tienes que seguir las instrucciones. Esto no es un espectáculo independiente, sino que necesita un presentador pero es profesionalmente producida y sonido hechos. Si usted decide usar el programa le enviaré una copia gratuita de mi libro electrónico, “Cómo obtener un pie” O “que le ayudará con habilidades de presentación. Sólo tiene que escribir a bob@baronson.org y por lo general usted recibirá una copia del mismo día.
Además … hay más información sobre este sitio de blogs sobre otros donación / trasplante temas. Además nos encantaría que te unas a nuestro grupo de Facebook, la Iniciativa de Trasplante de Órganos Cuantos más miembros que obtenemos mayor será nuestra influencia con los tomadores de decisiones.
To Remember Me — A Donor’s Request
To Remember Me
By Robert Noel Test (1926-1994)
The day will come when my body will lie upon a white sheet neatly tucked under four corners of a mattress located in a hospital; busily occupied with the living and the dying.
At a certain moment a doctor will determine that my brain has ceased to function and that, for all intents and purposes, my life has stopped. When that happens, do not attempt to instill artificial life into my body by the use of a machine. And don’t call this my deathbed. Let it be called the bed of life, and let my body be taken from it to help others lead fuller lives.
- Give my sight to the man who has never seen a sunrise, a baby’s face or love in the eyes of a woman.
- Give my heart to a person whose own heart has caused nothing but endless days of pain.
- Give my blood to the teenager who was pulled from the wreckage of his car, so that he might live to see his grandchildren play.
- Give my kidneys to the one who depends on a machine to exist from week to week.
- Take my bones, every muscle, every fiber and nerve in my body and find a way to make a crippled child walk.
- Explore every corner of my brain.
- Take my cells, if necessary, and let them grow so that, someday a speechless boy will shout at the crack of a bat and a deaf girl will hear the sound of rain against her window.
- Burn what is left of me and scatter the ashes to the winds to help the flowers grow.
- If you must bury something, let it be my faults, my weakness and all prejudice against my fellow man….
- If, by chance, you wish to remember me, do it with a kind deed or word to someone who needs you.
If you do all I have asked, I will live forever.
Bob Aronson is a 2007 heart transplant recipient, the founder of Facebook’s 1700 member Organ Transplant Initiative and the writer of most of these donation/transplantation blogs on Bob’s Newheart.
You may comment in the space provided or email your thoughts to me at bob@baronson.org. And – please spread the word about the immediate need for more organ donors. There is nothing you can do that is of greater importance. If you convince one person to be an organ and tissue donor you may save or positively affect over 60 lives. Some of those lives may be people you know and love.
Please view our video “Thank You From the Bottom of my Donor’s heart” on http://www.organti.org This video was produced to promote organ donation so it is free and no permission is needed for its use.
If you want to spread the word personally about organ donation, we have a PowerPoint slide show for your use free and for use without permission. Just go to http://www.organti.org and click on “Life Pass It On” on the left side of the screen and then just follow the directions. This is NOT a stand-alone show, it needs a presenter but is professionally produced and factually sound.
Also…there is more information on this blog site about other donation/transplantation issues. Additionally we would love to have you join our Facebook group, Organ Transplant Initiative The more members we get the greater our clout with decision makers.
Can Cellular Memory Cause Transplant Recipients to Act Like Their Donors?
I have been writing these blogs for almost five years. All of them are related to organ and tissue transplants and they range from how alcohol and drugs affect your organs to eating disorders, post transplant depression, mandatory donation and the Vice President Cheney Heart Transplant. None of them, though, have gotten anywhere near the response of the posts I’ve written about Cellular memory, the theory that certain cells in the body have memories of their own and that when transplanted into another person become the new person’s memories as well.
Personally I don’t put much stock in the claims of cellular memory but a lot of people do so who am I to say they are wrong especially when I get so many requests for more information on the subject … so here’s the latest I could dig up.
While many scientists will tell you that cellular memory is impossible there really isn’t very much science on the subject. Studies have been small and rare so while there is a lot of scientific doubt there is no absolute proof that the phenomenon does not exist.
Most doctors attribute the sometimes seismic personality changes after a transplant to radical health improvements, heavy doses of anesthesia and anti-rejection medications and psychological factors.
Like others University of Arizona psychologist Gary Schwartz has little real evidence to back up his theory that since every cell in the body contains a complete set of genetic material, transplant patients inherit DNA from their donors that determines, in part, how a person thinks, behaves and even eats. “Hearts can have memory, as brains do,” says Schwartz. Most doctors, however, say that’s the stuff of the Sci-Fi Channel and note that Schwartz based his theory on a study of just 10 transplant patients. “There is no evidence of clinical findings to suggest that [cellular memory exists],” says Dr. Tracy Stevens, medical director of the cardiac transplant program at St. Luke’s Hospital in Kansas City, Mo. You can read more here http://www.people.com/people/archive/article/0,,20147267,00.html
While medical and other scientific researchers will tell you that a truly scientific study would take years among perhaps hundreds of people there are some unexplainable individual cases. One of which is the story of Claire Sylvia who got a heart and lung transplant in the 1970s from an eighteen year old male who had died in a motorcycle accident. Ms. Sylvia knew oone of this information but claimed upon awakening that she had a new and intense craving for beer, chicken nuggets, and green peppers, all food she didn’t enjoy prior to the surgery. A change in food preferences is probably the most noted in heart transplant patients. Sylvia wrote a book about her experiences after learning the identity of her donor called A Change of Hear. You can watch her video here http://www.youtube.com/watch?v=OIDwRnBcrGw
And…if the Claire Sylvia story is not enough, here is yet another about a young woman, Julie Shambra in England who after suffering from diabetes for many years got a life saving transplant from a young man that changed her life and many of her habits and tastes. http://www.youtube.com/watch?v=NVVk3zAz8Qo&feature=related
The most stunning example of cellular memory was found in an eight year old girl who received the heart of a ten year old girl. The recipient was plagued after surgery with vivid nightmares about an attacker and a girl being murdered. After being brought to a psychiatrist her nightmares proved to be so vivid and real that the psychiatrist believed them to be genuine memories. As it turns out the ten year old whose heart she had just received was murdered and due to the recipients violent reoccurring dreams she was able to describe the events of that horrible encounter and the murderer so well that police soon apprehended, arrested, and convicted the killer. Unfortunately I have been unable to find out where or when this happened so there is no real proof that the story is anything more than an urban myth.
But then there are these stories:
Bill Wohl was a hard-driving self-described type A executive until cardiac disease nearly killed him in 2000. A heart transplant at the University of Arizona medical center saved his life—and transformed it in ways he could never have imagined. Weeks after his operation, Wohl, now 58, heard a song on the radio by the British vocalist Sade. “I just started crying and rocking,” he recalls. Odd, since before the surgery, Wohl hadn’t heard of Sade and was not the type to mist up over a torch song. Later he contacted the family of organ donor Michael Brady, the 36-year-old Hollywood stuntman whose heart he had received, and made an intriguing discovery. Sade was one of Brady’s favorite singers. “It was,” says Wohl, “really, really freaky.”
And then there is Paul Oldam, a corporate executive in a Milwaukee law firm, received the heart of a 14-year-old boy who had been killed in a truck accident in 1993. On Oldam’s first post-surgery shopping trip, his wife, Peggy, was taken aback when he wandered into the candy aisle and started loading the basket with Snickers bars. “He never liked candy before that,” Peggy says other husband, now 70. Bill also became an avid outdoorsman, given to kayaking, cross-country skiing and cycling 25 miles at a stretch. “I wouldn’t be surprised,” says Peggy, 69, “if he wanted to try parachuting next year.”
How Cellular Memory Might Work
It is thought that cellular memory might be possible since the discovery that neuropeptides exist not only in the brain as once thought but in all the tissues of the body. These neuropeptides are a way for the brain to “speak” to other bodily organs and for the organs to rely information back. However it is unknown if these newly found circuits could indeed store memories as the brain does in different organs. Due to the amount of peptides in the heart this organ is seen to have special potential in the study of this phenomena. However many answers still remain. Why don’t all transplant recipients have these experiences? It’s been theorized this may be due to the fact not all of them are in tune with their body as some other individuals may be. Perhaps the explanation lies with the sensitivity of the individual.
According to a story in Hub Pages which is not exactly a respected medical journal there are three possible explanations for cellular memory http://theophanes.hubpages.com/hub/Cellular-Memories-in-Organ-Transplant-Recipients
- The Hospital Grapevine Theory: The hospital grapevine theory is the simplest alternate explanation, stating that patients may be influenced due to information they hear from nurses talking to each other or their surgeons while they are under anesthesia. Although it’s forbidden to tell a transplant recipients the identity of the donor or any personal information there’s no such rule that prevents hospital staff from talking amongst themselves. Could all these coincidences be a placebo effect given to the highly suggestible?
- The Quantum Theory: this theory claims that the answers may lie in a world we are as of yet are very ill-equipped to prove, in the wonderfully strange world of quantum mechanics. Quantum mechanics tries to explain mathematically events that occur with atoms and the particles which may make up atoms. This is world where regular physics comes to die and can be used loosely to explain virtually anything that can’t be explained otherwise. It’s tempting but I’ll leave this one up to the mathematicians to toy with. As of yet I haven’t heard of any of them proposing this theory, it seems to be something thrown out there by laymen.
- The Drug Theory: It is the body’s duty to protect itself from foreign objects and that is generally what it does when it receives organs that weren’t grown in it from conception. This is why patients have to receive immunosuppressant drugs to stop their own bodies from attacking the new organ. There have only been a small handful of cases of people who have lived without these drugs, and they have done so on their own against the advice of doctors. this theory states that these drugs can be the cause of the changes in personality. Perhaps in some strange way these drugs can be psychoactive as well as immunosuppressive. This theory probably chalks up the specific nature of the said changes in personality to coincidence.
There is no definitive evidence one way or another that cellular memory exists. I can only speak for myself but I had a heart transplant almost five years ago and have absolutely no change in my personality or lifestyle at all. I am more appreciative of life than ever before but I think that might be true of anyone who was dying and had their life saved by a total stranger.
So we’ll close with the now well-known line, “We report… you decide.
Bob Aronson is a 2007 heart transplant recipient, the founder of Facebook’s 1700 member Organ Transplant Initiative and the writer of these donation/transplantation blogs on Bob’s Newheart.
You may comment in the space provided or email your thoughts to me at bob@baronson.org. And – please spread the word about the immediate need for more organ donors. There is nothing you can do that is of greater importance. If you convince one person to be an organ and tissue donor you may save or positively affect over 60 lives. Some of those lives may be people you know and love.
Please view our video “Thank You From the Bottom of my Donor’s heart” on http://www.organti.org This video was produced to promote organ donation so it is free and no permission is needed for its use.
If you want to spread the word personally about organ donation, we have a PowerPoint slide show for your use free and for use without permission. Just go to http://www.organti.org and click on “Life Pass It On” on the left side of the screen and then just follow the directions. This is NOT a stand-alone show, it needs a presenter but is professionally produced and factually sound.
Also…there is more information on this blog site about other donation/transplantation issues. Additionally we would love to have you join our Facebook group, Organ Transplant Initiative The more members we get the greater our clout with decision makers.



You must be logged in to post a comment.